Introduction :-
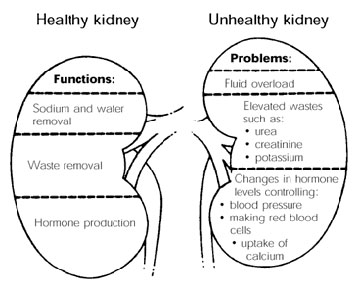
- Renal failure (also kidney failure or renal insufficiency) is a medical condition in which the kidneys fail to adequately filter waste products from the blood.
- The two main forms are acute kidney injury, which is often reversible with adequate treatment, and chronic kidney disease, which is often not reversible.
- Renal failure is mainly determined by a decrease in glomerular filtration rate, the rate at which blood is filtered in the glomeruli of the kidney. This is detected by adecrease in or absence of urine production or determination of waste products (creatinine or urea) in the blood. Depending on the cause, hematuria (blood loss in the urine) and proteinuria (protein loss in the urine) may be noted.
- In renal failure, there may be problems with increased fluid in the body (leading to swelling), increased acid levels, raised levels of potassium, decreased levels of calcium, increased levels of phosphate, and in later stages anemia. Bone health may also be affected. Long-term kidney problems are associated with an increased risk of cardiovascular disease.
Acute kidney injury
Pathologic kidney specimen showing marked pallor of the cortex, contrasting to the darker areas of surviving medullary tissue. The patient died with acute kidney injury.
- Acute kidney injury (AKI), previously called acute renal failure (ARF), is an abrupt loss of kidney function that develops within 7 days.
- Its causes are numerous. Generally it occurs because of damage to the kidneytissue caused by decreased renal blood flow (renal ischemia) from any cause (e.g. low blood pressure), exposure to substances harmful to the kidney, aninflammatory process in the kidney, or an obstruction of the urinary tract which impedes the flow of urine. AKI is diagnosed on the basis of characteristic laboratory findings, such as elevated blood urea nitrogen and creatinine, orinability of the kidneys to produce sufficient amounts of urine.
- AKI may lead to a number of complications, including metabolic acidosis, high potassium levels, uremia, changes in body fluid balance, and effects to otherorgan systems. Management includes supportive care, such as renal replacement therapy, as well as treatment of the underlying disorder.
Chronic kidney disease
Uremic frost on the forehead and scalp of a young man who presented with complaints of chronic anorexia and fatigue with blood urea nitrogen and serum creatinine levels of approximately 100 and 50 mg/dL respectively.
- Chronic kidney disease (CKD), also known as chronic renal disease (CRD), is a progressive loss in renal function over a period of months or years.
- The symptoms of worsening kidney function are non-specific, and might include feeling generally unwell and experiencing a reduced appetite.
- Often, chronic kidney disease is diagnosed as a result of screening of people known to be at risk of kidney problems, such as those with high blood pressure or diabetes and those with a blood relative with chronic kidney disease.
- Chronic kidney disease may also be identified when it leads to one of its recognized complications, such as cardiovascular disease, anemia or pericarditis.
- It is differentiated from acute kidney disease in that the reduction in kidney function must be present for over 3 months.
- Chronic kidney disease is identified by a blood test for creatinine. Higher levels of creatinine indicate a lower glomerular filtration rate and as a result a decreased capability of the kidneys to excrete waste products. Creatinine levels may be normal in the early stages of CKD, and the condition is discovered ifurinalysis (testing of a urine sample) shows that the kidney is allowing the loss ofprotein or red blood cells into the urine. To fully investigate the underlying cause of kidney damage, various forms of medical imaging, blood tests and often renalbiopsy (removing a small sample of kidney tissue) are employed to find out if there is a reversible cause for the kidney malfunction. Recent professional guidelines classify the severity of chronic kidney disease in five stages, with stage 1 being the mildest and usually causing few symptoms and stage 5 being a severe illness with poor life expectancy if untreated. Stage 5 CKD is often called end stage renal disease (ESRD), end stage renal failure (ESRF), or end-stage kidney disease (ESKD) and is synonymous with the now outdated terms chronic kidney failure (CKF) or chronic renal failure (CRF).
- There is no specific treatment unequivocally shown to slow the worsening of chronic kidney disease. If there is an underlying cause to CKD, such as vasculitis, this may be treated directly to slow the damage. In more advanced stages, treatments may be required for anemia and bone disease. Severe CKD requires renal replacement therapy, which may involve a form of dialysis, but ideally constitutes a kidney transplant.
Acute-on-chronic renal failure
- Acute kidney injuries can be present on top of chronic kidney disease, a condition called acute-on-chronic renal failure (AoCRF). The acute part of AoCRF may be reversible, and the goal of treatment, as with AKI, is to return the patient to baseline renal function, typically measured by serum creatinine. Like AKI, AoCRF can be difficult to distinguish from chronic kidney disease if the patient has not been monitored by a physician and no baseline (i.e., past) blood work is available for comparison.
Symptoms can vary from person to person. Someone in early stage kidney disease may not feel sick or notice symptoms as they occur. When kidneys fail to filter properly, waste accumulates in the blood and the body, a condition called azotemia. Very low levels of azotaemia may produce few, if any, symptoms. If the disease progresses, symptoms become noticeable (if the failure is of sufficient degree to cause symptoms). Renal failure accompanied by noticeable symptoms is termed uraemia.
Symptoms of kidney failure include the following :-
- High levels of urea in the blood, which can result in:
- Vomiting and/or diarrhea, which may lead to dehydration
- Nausea
- Weight loss
- Nocturnal urination
- More frequent urination, or in greater amounts than usual, with pale urine
- Less frequent urination, or in smaller amounts than usual, with dark coloured urine
- Blood in the urine
- Pressure, or difficulty urinating
- Unusual amounts of urination, usually in large quantities
- A buildup of phosphates in the blood that diseased kidneys cannot filter out may cause:
- Itching
- Bone damage
- Nonunion in broken bones
- Muscle cramps (caused by low levels of calcium which can be associated with hyperphosphatemia)
- A buildup of potassium in the blood that diseased kidneys cannot filter out (called hyperkalemia) may cause:
- Abnormal heart rhythms
- Muscle paralysis
- Failure of kidneys to remove excess fluid may cause:
- Swelling of the legs, ankles, feet, face and/or hands
- Shortness of breath due to extra fluid on the lungs (may also be caused by anemia)
- Polycystic kidney disease, which causes large, fluid-filled cysts on the kidneys and sometimes the liver, can cause:
- Pain in the back or side
- Healthy kidneys produce the hormone erythropoietin that stimulates the bone marrow to make oxygen-carrying red blood cells. As the kidneys fail, they produce less erythropoietin, resulting in decreased production of red blood cells to replace the natural breakdown of old red blood cells. As a result, the blood carries less hemoglobin, a condition known as anemia. This can result in:
- Feeling tired and/or weak
- Memory problems
- Difficulty concentrating
- Dizziness
- Low blood pressure
- Normally, proteins are too large to pass through the kidneys, however, they are able to pass through when the glomeruli are damaged. This does not cause symptoms until extensive kidney damage has occurred, after which symptoms include:
- Foamy or bubbly urine
- Swelling in the hands, feet, abdomen, or face
- Other symptoms include:
- Appetite loss, a bad taste in the mouth
- Difficulty sleeping
- Darkening of the skin
- Excess protein in the blood
- With high dose penicillin, renal failure patients may experience seizures
Causes :-
Acute kidney injury
- Acute kidney injury (previously known as acute renal failure) - or AKI - usually occurs when the blood supply to the kidneys is suddenly interrupted or when the kidneys become overloaded with toxins. Causes of acute kidney injury include accidents, injuries, or complications from surgeries in which the kidneys are deprived of normal blood flow for extended periods of time. Heart-bypass surgery is an example of one such procedure.
- Drug overdoses, accidental or from chemical overloads of drugs such as antibiotics or chemotherapy, may also cause the onset of acute kidney injury. Unlike chronic kidney disease, however, the kidneys can often recover from acute kidney injury, allowing the patient to resume a normal life. People suffering from acute kidney injury require supportive treatment until their kidneys recover function, and they often remain at increased risk of developing future kidney failure.
- Among the accidental causes of renal failure is the crush syndrome, when large amounts of toxins are suddenly released in the blood circulation after a long compressed limb is suddenly relieved from the pressure obstructing the blood flow through its tissues, causing ischemia. The resulting overload can lead to the clogging and the destruction of the kidneys. It is areperfusion injury that appears after the release of the crushing pressure. The mechanism is believed to be the release into the bloodstream of muscle breakdown products – notably myoglobin, potassium, and phosphorus – that are the products of rhabdomyolysis (the breakdown of skeletal muscle damaged by ischemic conditions). The specific action on the kidneys is not fully understood, but may be due in part to nephrotoxic metabolites of myoglobin.
Chronic kidney disease
- Chronic Kidney Disease (CKD) has numerous causes. The most common causes of CKD are diabetes mellitus and long-term, uncontrolled hypertension. Polycystic kidney disease is another well-known cause of CKD. The majority of people afflicted with polycystic kidney disease have a family history of the disease. Other genetic illnesses affect kidney function, as well.
- Overuse of common drugs such as aspirin, ibuprofen, and acetaminophen (paracetamol) can also cause chronic kidney damage.
- Some infectious diseases, such as hantavirus, can attack the kidneys, causing kidney failure.
Genetic predisposition
- The APOL1 gene has been proposed as a major genetic risk locus for a spectrum of nondiabetic renal failure in individuals of African origin, these include HIV-associated nephropathy (HIVAN), primary nonmonogenic forms of focal segmental glomerulosclerosis, and hypertension affiliated chronic kidney disease not attributed to other etiologies. Two western African variants in APOL1 have been shown to be associated with end stage kidney disease in African Americans and Hispanic Americans.
Diagnostic Approach :-
Measurement for AKI
Acute kidney injury is diagnosed on the basis of clinical history and laboratory data. A diagnosis is made when there is rapid reduction in kidney function, as measured by serum creatinine, or based on a rapid reduction in urine output, termed oliguria.
Classic laboratory findings in AKI
Type UOsm UNa FeNa BUN/Cr Prerenal >500 <10 <1% >20 Intrinsic <350 >20 >2% <15 Postrenal <350 >40 >4% >15
Definition
Introduced by the KDIGO in 2012, specific criteria exist for the diagnosis of AKI.
AKI can be diagnosed if any one of the following is present:
- Increase in SCr by ≥0.3 mg/dl (≥26.5 μmol/l) within 48 hours; or
- Increase in SCr to ≥1.5 times baseline, which have occurred within the prior 7 days; or
- Urine volume < 0.5 ml/kg/h for 6 hours.
Staging
The RIFLE criteria, proposed by the Acute Dialysis Quality Initiative (ADQI) group, aid in the staging of patients with AKI:
- Risk: 1.5-fold increase in the serum creatinine, or glomerular filtration rate (GFR) decrease by 25 percent, or urine output <0.5 mL/kg per hour for six hours.
- Injury: Twofold increase in the serum creatinine, or GFR decrease by 50 percent, or urine output <0.5 mL/kg per hour for 12 hours
- Failure: Threefold increase in the serum creatinine, or GFR decrease by 75 percent, or urine output of <0.3 mL/kg per hour for 24 hours, or anuria for 12 hours
- Loss: Complete loss of kidney function (e.g., need for renal replacement therapy) for more than four weeks
- End-stage renal disease: Complete loss of kidney function (e.g., need for renal replacement therapy) for more than three months
Measurement for CKD
- Stages of kidney failure
- Chronic kidney failure is measured in five stages, which are calculated using a patient’s GFR, or glomerular filtration rate.
- Stage 1 CKD is mildly diminished renal function, with few overt symptoms.
- Stages 2 and 3 need increasing levels of supportive care from their medical providers to slow and treat their renal dysfunction.
- Patients in stages 4 and 5 usually require preparation of the patient towards active treatment in order to survive. Stage 5 CKD is considered a severe illness and requires some form of renal replacement therapy (dialysis) or kidney transplant whenever feasible.
- Glomerular filtration rate
CKD Stage GFR level (mL/min/1.73 m2) Stage 1 ≥ 90 Stage 2 60 – 89 Stage 3 30 – 59 Stage 4 15 – 29 Stage 5 < 15
- A normal GFR varies according to many factors, including sex, age, body size and ethnic background. Renal professionals consider the glomerular filtration rate (GFR) to be the best overall index of kidney function. The National Kidney Foundation offers an easy to use on-line GFR calculator for anyone who is interested in knowing their glomerular filtration rate. (A serum creatinine level, a simple blood test, is needed to use the calculator).
Use of the term uremia
- Before the advancement of modern medicine, renal failure was often referred to as uremic poisoning. Uremia was the term for the contamination of the blood with urine. It is the presence of an excessive amount of urea in blood. Starting around 1847, this included reduced urine output, which was thought to be caused by the urine mixing with the blood instead of being voided through the urethra. The term uremia is now used for the illness accompanying kidney failure.
Management :-
In Morden Medicine
- The management of AKI hinges on identification and treatment of the underlying cause. In addition to treatment of the underlying disorder, management of AKI routinely includes the avoidance of substances that are toxic to the kidneys, called nephrotoxins. These include NSAIDs such as ibuprofen, iodinated contrasts such as those used for CT scans, many antibiotics such as gentamicin, and a range of other substances.
- Monitoring of renal function, by serial serum creatinine measurements and monitoring of urine output, is routinely performed. In the hospital, insertion of a urinary catheter helps monitor urine output and relieves possible bladder outlet obstruction, such as with an enlarged prostate.
Specific therapies
- In prerenal AKI without fluid overload, administration of intravenous fluids is typically the first step to improve renal function. Volume status may be monitored with the use of a central venous catheter to avoid over- or under-replacement of fluid.
- Should low blood pressure prove a persistent problem in the fluid-replete patient, inotropes such as norepinephrine anddobutamine may be given to improve cardiac output and hence renal perfusion. While a useful pressor, there is no evidence to suggest that dopamine is of any specific benefit, and may be harmful.
- The myriad causes of intrinsic AKI require specific therapies. For example, intrinsic AKI due to Wegener's granulomatosismay respond to steroid medication. Toxin-induced prerenal AKI often responds to discontinuation of the offending agent, such as aminoglycoside, penicillin, NSAIDs, or paracetamol.
- If the cause is obstruction of the urinary tract, relief of the obstruction (with a nephrostomy or urinary catheter) may be necessary.
Diuretic agents
- The use of diuretics such as furosemide, is widespread and sometimes convenient in ameliorating fluid overload. It is not associated with higher mortality (risk of death), nor with any reduced mortality or length of intensive care unit or hospital stay.
Renal replacement therapy
- Renal replacement therapy, such as with hemodialysis, may be instituted in some cases of AKI. A systematic review of the literature in 2008 demonstrated no difference in outcomes between the use of intermittent hemodialysis and continuous venovenous hemofiltration (CVVH). Among critically ill patients, intensive renal replacement therapy with CVVH does not appear to improve outcomes compared to less intensive intermittent hemodialysis.
A hemodialysis machine, used to physiologically aid or replace the kidneys in renal failure
Treatment in Homoeopathy :-
" One Single Simple Drug Substance In Its Most Suitable Potency, According To Symptom Similarity Based On Totality! "
Aconite
Incipient stage of post scarlatinal nephritis, pain in loins, scanty urine without blood.
Apis mellifica
Apis is not so much a remedy for chronic Bright’s disease as for the acuter forms. There are oedematous swellings of the face and extremities, paleness, ascites, oedema pulmonum, pains in the head, back and limbs. Albuminuria following scarlatina. It may be of use in any form of Bright’s disease when there are dull pains in the kidneys, scanty urine and frequent Micturition. The urine is heavily charged with albumen and contains blood corpuscles. The oedema appears quickly, there is general dropsy and suppression of urine and perhaps an eruption of the skin like a nettle rash. The patient is drowsy, apathetic and has a bruised feeling all over. Apis in such cases acts best in trituration; do not depend on the tincture or dilutions. Hepar is recommended by Kafka in Bright’s disease following scarlatina. A valuable symptom for Apis is the feeling of suffocation. He does not see how he is get another breath.
Apocynum
Palliative in dropsical conditions where the urine is scanty. Also useful for coma & convulsions in the nephritis of pregnency.
Arsenicum
This remedy corresponds to all stages of Bright’s disease, bearing a closer resemblance than any other remedy. It comes in later in the disease where there is dropsy, pale skin, waxen appearance, watery diarrhea and great thirst. The urine is dark, casts are abundant, and it contains much albumen. There are attacks of dyspnoea when lying down in the evening and after midnight, relieved by an expectoration of mucus. It may come in immediately after Aconite in many cases. “Blood boils” make a special indication for this remedy. Baehr, Millard and Hale question the usefulness of Arsenicum in kidney affections. However, it seems a simile to the large white kidney; in fact, one could hardly wish for a closer correspondence. Hughes considers it a favorite with anxiety and sinking of vital forces will call for Arsenicum. Calcarea arsenica has been used in the anaemia, progressive emaciation and debility of this disease with success.
Aurum muriaticum
Morbus Brightii from gout, suppurations or syphilis. Interstitial nephritis in its incipiency with digestive and nervous phenomena, hypochondriasis, irritability and vertigo.
Belladonna
Simple albuminuria, here it seems to occupy a place midway between Aconite and Arsenicum. Belladonna is of the greatest service in inflammation of the kidneys with piercing burning pains in the lumbar region, returning periodically with increased severity.
Cantharis
This remedy pictures nephritis with cutting pains in the lumbar region; the urine is passed in drops and is mixed with blood, with much urging. Post scarlatinal and post diphtheric kidney diseases with dropsy may indicate Cantharis.
Convallaria
Nephritis from heart disorders. It affords relief when there is extreme rapid & irregular action of the heart, and in general anasarca & ascites from mitral insufficiency.
Cuprum arsenicum
Cuprum arsenicum is also useful in uraemic conditions and is praised highly by Goodno. Cuprum is a valuable remedy for uraemic eclampsia.
Digitalis
This remedy has an irritant action on the kidneys. It is homoeopathic to granular degeneration. Heart symptoms, feeble pulse, scanty, dark, turbid urine, faintness at the stomach, rheumatic pains will indicate it. It is especially useful when the circulation is weak. Rheumatic pains, pulmonary catarrh with profuse expectoration are marked symptoms.
Glonoine
Glonoine has albuminous urine and will sometimes be found useful in acute and haemorrhagic nephritis.
Kali chloricum
This remedy is said to be the most homoeopathic of all remedies in Bright’s disease. It has scanty, dark, albuminous urine containing casts. It excites a violent nephritis.
Mercurius corrosivus
This remedy corresponds to the large white kidney. There is an albuminous, scanty and red urine; pale waxen color of the body; there are lumbar pains, great dyspnoea and excessive strangury. It takes the first rank among all the mercurials for nephritis, and it comes in the later stages. Syphilitic complication further indicate it. There is an expression of uneasiness on the face. Dr. Ludlam considers it our best remedy for the albuminous nephritis of pregnancy and Baehr lauds it in suppurative nephritis.
Plumbum
Granular degenerations of the kidneys, with tendency to uraemic convulsion. Dropsy, sallow face, emaciation, oedema about the ankles. It seems to corresponds to the contracted or cirrhotic form of nephritis, holding the same relation here that Arsenic and Mercury do in chronic nephritis. Royal emphasizes this remedy saying that it arrested the progress in many cases and permanently cured not few for him.
Phosphorus
Phosphorus produces as marked a nephritis as any drug. It is one of the most important remedies in Bright’s disease; the characteristic symptoms are: lassitude of the whole body, hands and feet icy cold, sleepiness. The fatigue is greatest in the morning, and there is heat in the body without thirst, especially in the evening. The patient is indisposed to work, is giddy, forgetful and has a heavy headache, particularly in the forehead; there is oedema of the upper eyelids, a mist before the eye, a yellowish fray complexion, a sickly oedema of the face, want of appetite, pressure and burning in the stomach, and a light colored painless diarrhea which is very weakening. It suits well fatty or waxy casts, is dark brown, scanty and albuminous, or covered with an iridescent film. Pulmonary complications will call for Phosphorus; and inability to lie on the left side is a prominent symptom in these cases. Vomiting and gastric symptoms are usually present. A small dose of Phosphorus will act much safer and better in eclampsia than a large dose of Morphine.
Terebinth
One of our reliable and most frequently indicated remedies in the early stages of renal diseases when congestion is prominent, when there is much pain in the back of a dull character extending along the ureters. The great characteristic of dark smoky urine will be present. There is anasarca, and of course, the urine is bloody and albuminous. It is recommended in post scarlatinal renal affections. The prostration is not accompanied by the restlessness of Arsenicum.
Incipient stage of post scarlatinal nephritis, pain in loins, scanty urine without blood.
Apis mellifica
Apis is not so much a remedy for chronic Bright’s disease as for the acuter forms. There are oedematous swellings of the face and extremities, paleness, ascites, oedema pulmonum, pains in the head, back and limbs. Albuminuria following scarlatina. It may be of use in any form of Bright’s disease when there are dull pains in the kidneys, scanty urine and frequent Micturition. The urine is heavily charged with albumen and contains blood corpuscles. The oedema appears quickly, there is general dropsy and suppression of urine and perhaps an eruption of the skin like a nettle rash. The patient is drowsy, apathetic and has a bruised feeling all over. Apis in such cases acts best in trituration; do not depend on the tincture or dilutions. Hepar is recommended by Kafka in Bright’s disease following scarlatina. A valuable symptom for Apis is the feeling of suffocation. He does not see how he is get another breath.
Apocynum
Palliative in dropsical conditions where the urine is scanty. Also useful for coma & convulsions in the nephritis of pregnency.
Arsenicum
This remedy corresponds to all stages of Bright’s disease, bearing a closer resemblance than any other remedy. It comes in later in the disease where there is dropsy, pale skin, waxen appearance, watery diarrhea and great thirst. The urine is dark, casts are abundant, and it contains much albumen. There are attacks of dyspnoea when lying down in the evening and after midnight, relieved by an expectoration of mucus. It may come in immediately after Aconite in many cases. “Blood boils” make a special indication for this remedy. Baehr, Millard and Hale question the usefulness of Arsenicum in kidney affections. However, it seems a simile to the large white kidney; in fact, one could hardly wish for a closer correspondence. Hughes considers it a favorite with anxiety and sinking of vital forces will call for Arsenicum. Calcarea arsenica has been used in the anaemia, progressive emaciation and debility of this disease with success.
Aurum muriaticum
Morbus Brightii from gout, suppurations or syphilis. Interstitial nephritis in its incipiency with digestive and nervous phenomena, hypochondriasis, irritability and vertigo.
Belladonna
Simple albuminuria, here it seems to occupy a place midway between Aconite and Arsenicum. Belladonna is of the greatest service in inflammation of the kidneys with piercing burning pains in the lumbar region, returning periodically with increased severity.
Cantharis
This remedy pictures nephritis with cutting pains in the lumbar region; the urine is passed in drops and is mixed with blood, with much urging. Post scarlatinal and post diphtheric kidney diseases with dropsy may indicate Cantharis.
Convallaria
Nephritis from heart disorders. It affords relief when there is extreme rapid & irregular action of the heart, and in general anasarca & ascites from mitral insufficiency.
Cuprum arsenicum
Cuprum arsenicum is also useful in uraemic conditions and is praised highly by Goodno. Cuprum is a valuable remedy for uraemic eclampsia.
Digitalis
This remedy has an irritant action on the kidneys. It is homoeopathic to granular degeneration. Heart symptoms, feeble pulse, scanty, dark, turbid urine, faintness at the stomach, rheumatic pains will indicate it. It is especially useful when the circulation is weak. Rheumatic pains, pulmonary catarrh with profuse expectoration are marked symptoms.
Glonoine
Glonoine has albuminous urine and will sometimes be found useful in acute and haemorrhagic nephritis.
Kali chloricum
This remedy is said to be the most homoeopathic of all remedies in Bright’s disease. It has scanty, dark, albuminous urine containing casts. It excites a violent nephritis.
Mercurius corrosivus
This remedy corresponds to the large white kidney. There is an albuminous, scanty and red urine; pale waxen color of the body; there are lumbar pains, great dyspnoea and excessive strangury. It takes the first rank among all the mercurials for nephritis, and it comes in the later stages. Syphilitic complication further indicate it. There is an expression of uneasiness on the face. Dr. Ludlam considers it our best remedy for the albuminous nephritis of pregnancy and Baehr lauds it in suppurative nephritis.
Plumbum
Granular degenerations of the kidneys, with tendency to uraemic convulsion. Dropsy, sallow face, emaciation, oedema about the ankles. It seems to corresponds to the contracted or cirrhotic form of nephritis, holding the same relation here that Arsenic and Mercury do in chronic nephritis. Royal emphasizes this remedy saying that it arrested the progress in many cases and permanently cured not few for him.
Phosphorus
Phosphorus produces as marked a nephritis as any drug. It is one of the most important remedies in Bright’s disease; the characteristic symptoms are: lassitude of the whole body, hands and feet icy cold, sleepiness. The fatigue is greatest in the morning, and there is heat in the body without thirst, especially in the evening. The patient is indisposed to work, is giddy, forgetful and has a heavy headache, particularly in the forehead; there is oedema of the upper eyelids, a mist before the eye, a yellowish fray complexion, a sickly oedema of the face, want of appetite, pressure and burning in the stomach, and a light colored painless diarrhea which is very weakening. It suits well fatty or waxy casts, is dark brown, scanty and albuminous, or covered with an iridescent film. Pulmonary complications will call for Phosphorus; and inability to lie on the left side is a prominent symptom in these cases. Vomiting and gastric symptoms are usually present. A small dose of Phosphorus will act much safer and better in eclampsia than a large dose of Morphine.
Terebinth
One of our reliable and most frequently indicated remedies in the early stages of renal diseases when congestion is prominent, when there is much pain in the back of a dull character extending along the ureters. The great characteristic of dark smoky urine will be present. There is anasarca, and of course, the urine is bloody and albuminous. It is recommended in post scarlatinal renal affections. The prostration is not accompanied by the restlessness of Arsenicum.
& The List Goes On.....
Ultimately similimum can only be found by taking totality of the symptoms as per the individual case.
For More Details :-
Take Care Of Your Body,
It's The Only Place You Have To Live In.
With Best Regards, Karnav Thakkar :) :)













No comments:
Post a Comment